How to Submit a Claim
A Step-by-Step Guide to the Claims Process for Atlas Travel®, Atlas PremiumTM, Atlas Group®, Atlas MultiTripTM, Atlas NomadsTM, and StudentSecure® Members
We hope you find our updated claims guide useful and enjoy an improved experience with the launch of our Member Portal (formerly known as Client Zone / Student Zone).
Please note that this step-by-step guide applies to domestic and international claims submitted both in-network and out-of-network. Our claims department processes claims based on the terms and conditions described in your policy.
IMPORTANT! This guide applies only to Atlas Travel, Atlas Premium, Atlas Group, Atlas MultiTrip, Atlas Nomads, and Student Secure travel medical insurance plans. If you have an Atlas Journey® or Atlas On-The-Go™ trip protection insurance plan, please see the "Claims Process" section of our Trip Insurance FAQ page to learn about your claims process.
You can also find claims information for Atlas Journey and Atlas On-The-Go in the "Claim Provisions" section of the policy documents that we sent to your email upon purchase. Visit the Atlas Journey or Atlas On-The-Go product page to download another copy of your policy documents. Click the "Policy Documents" tab and use the dropdown to select your state. Then click the link for the policy you purchased.
Jump to Section:
- How the Claims Process Works
- How to File a Claim
- How the Direct Billing and Claims Reimbursement Process Work
- How the Claims Review Process Works
- How to View Your Claim Status and Navigate Member Portal (Formerly Known as Client Zone / Student Zone)
- How to Appeal a Claim
IMPORTANT! Member Portal (formerly known as Client Zone / Student Zone) is our new and improved online portal where policyholders can manage their WorldTrips insurance plans.
If you currently have a Client Zone or Student Zone account, there is no need to register for a Member Portal account. Simply enter your Client Zone / Student Zone details on the Member Portal welcome page to enjoy an improved experience.
-
Click to view instructions
- Present your insurance ID card to your medical provider at the time of service.
*Make sure you provide your name in the same format as provided for your insurance policy. You can see your insured name format on your ID card and fulfillment documents (these were sent to you upon purchase and can also be found in Member Portal).
- Unless you are required to pay for medical treatment at the time of service, your provider will submit your claim directly to WorldTrips.
- WorldTrips will send you a letter notifying you that we have received your claim.
- We will also request a Claimant’s Statement and Authorization form or other information from you. If we do not receive the information requested from you within 45 days, your claim may be closed.
Once the fully completed Claimant’s Statement and Authorization form is received, WorldTrips may request medical records from your billing providers and/or any medical provider.
*WorldTrips requests to receive this information from the provider(s) within 45 days of the original request.
*If medical records are requested, you may reach out to the billing provider(s) and/or medical provider(s) to obtain copies—or submit the records you collected at the time of service to WorldTrips. However, this is typically the provider’s responsibility.
- WorldTrips will complete the claims process once we have all the necessary information.
- If the claim is deemed eligible, WorldTrips will secure any preferred provider discounts (if applicable).
- Present your insurance ID card to your medical provider at the time of service.
If You're Required to Pay for Medical Treatment at the Time of Service
-
Click to view instructions
We encourage providers to bill us directly, rather than requiring immediate payment from you. While we are always willing to pay providers directly for eligible claims, we cannot guarantee that the provider will accept your proof of insurance at the time of service.
- Present your insurance ID card to your medical provider at the time of service.
*Make sure you provide your name in the same format as provided for your insurance policy. You can see your insured name format on your ID card and fulfillment documents (these were sent to you upon purchase and can also be found in Member Portal).
- Ask your medical provider for your complete medical records from the visit as well as the receipt for your payment. Request an itemized bill with the following information:
a. Provider name and address
b. Provider tax ID (if U.S.-based)
c. Your name, date of birth, and policy/certificate ID number
d. Itemized charges
e. DX (Diagnosis) code and CPT (Current Procedural Technology) code. These are the codes your physician’s office uses to tell our claims examiners which procedures, diagnoses, and services you received during your visit.
*Keep your medical records, receipts, and itemized bills.
- You must complete, sign, and submit the Claimant’s Statement and Authorization form for every incident. Once we receive the fully completed Claimant’s Statement and Authorization form, WorldTrips may request medical records from your billing providers and/or any medical provider.
*If medical records are requested, you may reach out to the billing provider(s) and/or medical provider(s) to obtain copies—or submit the records you collected at the time of service to WorldTrips. However, this is typically the provider’s responsibility.
*WorldTrips requests to receive this information from the provider(s) within 45 days of the original request.
- We will also request receipts, invoices, and/or itemized bills from you. You will have 45 days to send us the information.
*Be sure to keep a copy of all submitted documents for your records.
- WorldTrips will complete the claims process once we have all the necessary information.
- If the claim is deemed eligible, WorldTrips will secure any preferred provider discounts (if applicable).
- Present your insurance ID card to your medical provider at the time of service.
-
Click to view instructions
- Present your insurance ID card to your medical provider at the time of service.
*Make sure you provide your name in the same format as provided for your insurance policy. You can see your insured name format on your ID card and fulfillment documents (these were sent to you upon purchase and can also be found in Member Portal).
- Unless the provider will be billing WorldTrips directly, you will pay for treatment at the time of service.
- At the time of service, ask your medical provider for your complete medical records from the visit as well as the receipt for your payment.
Also request an itemized bill with the following information:
a. Provider name and address
b. Your name, date of birth, and certificate ID number
c. Itemized charges
d. DX (Diagnosis) code and CPT (Current Procedural Terminology) code (these are the codes your physician’s office uses to tell our claims examiners which procedures, diagnoses, and services you received during your visit)
*Keep your medical records, receipts, and itemized bills.
- You must complete, sign, and submit the Claimant’s Statement and Authorization form for every incident. Once we receive the fully completed Claimant’s Statement and Authorization form, WorldTrips may request medical records from your billing providers and/or any medical provider.
*If medical records are requested, you may reach out to your billing provider(s) and/or medical provider(s) to obtain copies—or submit the records you collected at the time of service to WorldTrips. However, this is typically the provider’s responsibility.
*WorldTrips requests to receive this information from the provider(s) within 45 days of the original request.
- We will also request receipts, invoices, and/or itemized bills from you. You will have 45 days to send us the information.
*Be sure to keep a copy of all submitted documents for your records.
- WorldTrips will complete the claims process once we have all the necessary information.
- Present your insurance ID card to your medical provider at the time of service.
How to File a Claim
To file a claim, you must complete, sign, and submit a Claimant's Statement and Authorization form along with supporting documents for every incident.
Important Note If You Are Filing This Claim on Behalf of Another Person
If you are filing this claim on behalf of another person, you MUST fill out the section of the Claimant's Statement and Authorization form labeled "Supplement D - Authorization Form for Use and/or Disclosure of Protected Health Information." (This section of the claim form is also referred to as a HIPAA form).
This section must be signed by the policyholder in order for us to speak with you regarding any of the policyholder's Protected Health Information (PHI). Without this signed form, we may only disclose to you the status of the claim.
Already Submitted Your Claim and Did Not Complete Supplement D?
You do not need to submit a whole new claim form. See your options for submitting the Authorization Form for Use and/or Disclosure of Protected Health Information (HIPAA form) separately here.
Important Note for Students
For eligibility purposes, you must submit the following along with a Claimant’s Statement and Authorization form:
- A copy of your education-related visa (F-1, J-1, OPT, etc.) or valid I-20/DS2019
- Proof of full-time student status (not necessary if submitting a valid F-1 visa including OPT, or J-1 visa)
If you have questions or need assistance, please call global customer support at (800) 605-2282.
Important Note Regarding Upfront Payments
If you paid for medical treatment upfront and wish to be reimbursed for an approved claim electronically, make sure you complete the appropriate section of the Claimant's Statement and Authorization form titled "Supplement C - Payment Authorization Agreement Form." If you do not make your selection and fill out the information for your preferred payment type, you will receive a paper check for reimbursement of any eligible expenses to the name and address listed on file.
If you have already submitted your claim and did not fill out the "Authorization Agreement Form - Wire Payments” section, you do not need to submit a whole new claim form. You may instead fill out and submit the Payment Authorization Agreement Form with your payment preference via DocuSign within Member Portal.
Sign in and click “Claims and Appeals” in the main navigation. Then click the “Fill Out and Submit Via DocuSign” button under the “Payment Forms” subheader in the “File a Claim” section.
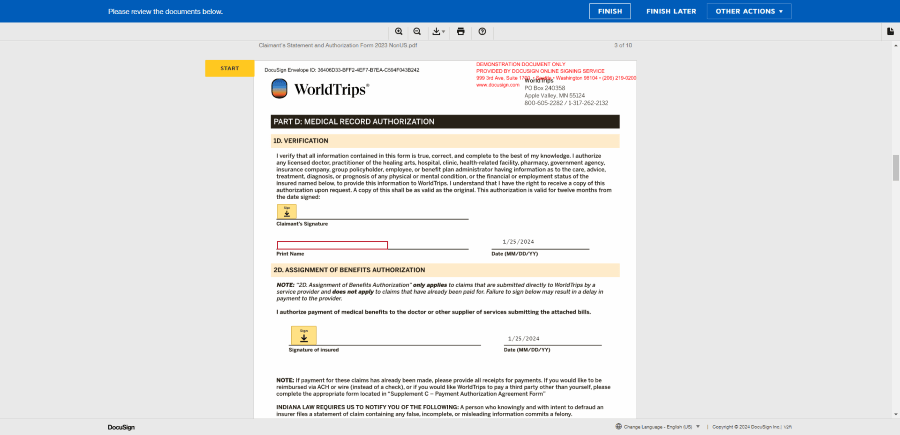
Enter your name and email address and click the “Begin Signing” button. Click the box next to “I agree to use electronic records and signatures.” Then click the yellow “Continue” button, select your preferred payment type, fill in the required information (as noted by the red boxes), sign the form, and click the yellow “Finish” button.
Clicking “Finish” submits your document and sends a PDF of your signed Payment Authorization Agreement Form to your email. Download or print a copy of your completed form for your records. If you do not receive a confirmation email with your completed form attached within 24 hours, please contact WorldTrips to make sure your form was properly submitted.
Don’t Have Access to the Claims and Appeals Page?
If you are not the insured or the insured’s legal guardian, you will see the Protected Health Information Authorization page in place of the Claims and Appeals page. Enter the insured’s email address and click “Send Request.” Once the insured has completed and submitted our HIPAA form, you will gain access to the Claims and Appeals page within 3-5 days.
You can complete and submit the Claimant's Statement and Authorization form and supporting documents in one of the following ways:
-
Click to view instructions
You can complete, sign, and submit the Claimant’s Statement and Authorization form online via Member Portal, our self-service portal for policyholders.
But First, Did You Register for a Member Portal Account?
To access Member Portal, you will first need to register an account. Please refer to the "How to Register for a Member Portal Account" section of this document for registration instructions.
If you have already registered your account, follow the instructions below.
If you have an existing Client Zone or Student Zone account, you do not need to register for Member Portal. Simply sign into Member Portal using your Client Zone or Student Zone log in information.
Haven’t Yet Added Your Policy to Your Member Portal Account?
You will need to add your policy to your Member Portal account before you will be able to submit a claim via Member Portal. Click here to jump to the “How to Add a Policy to Member Portal” section of this guide.
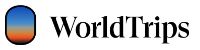
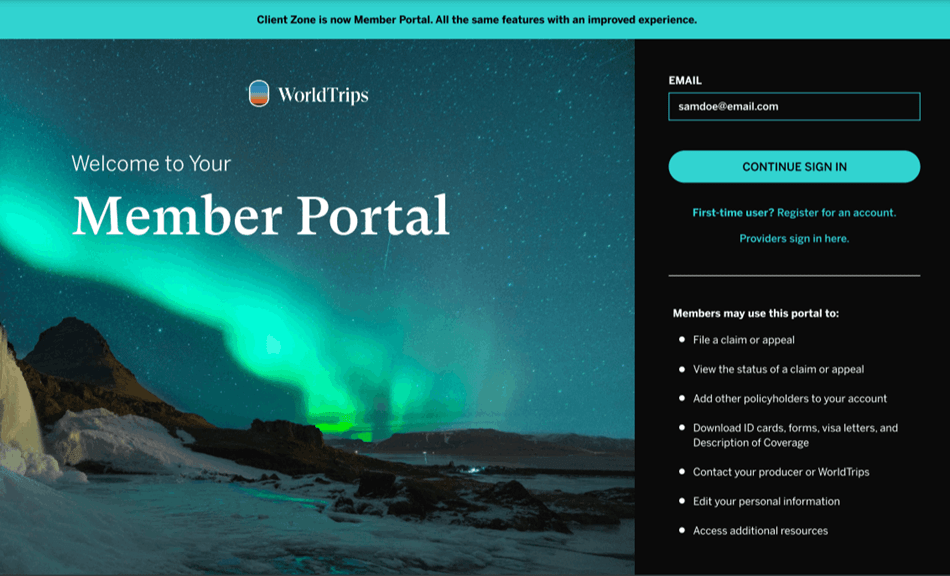
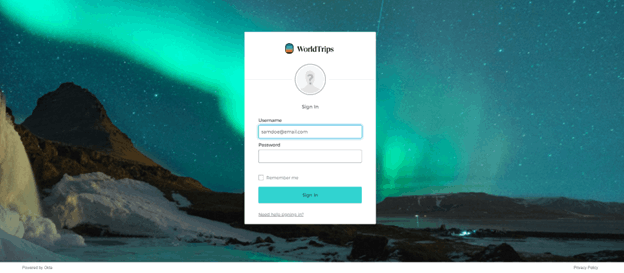
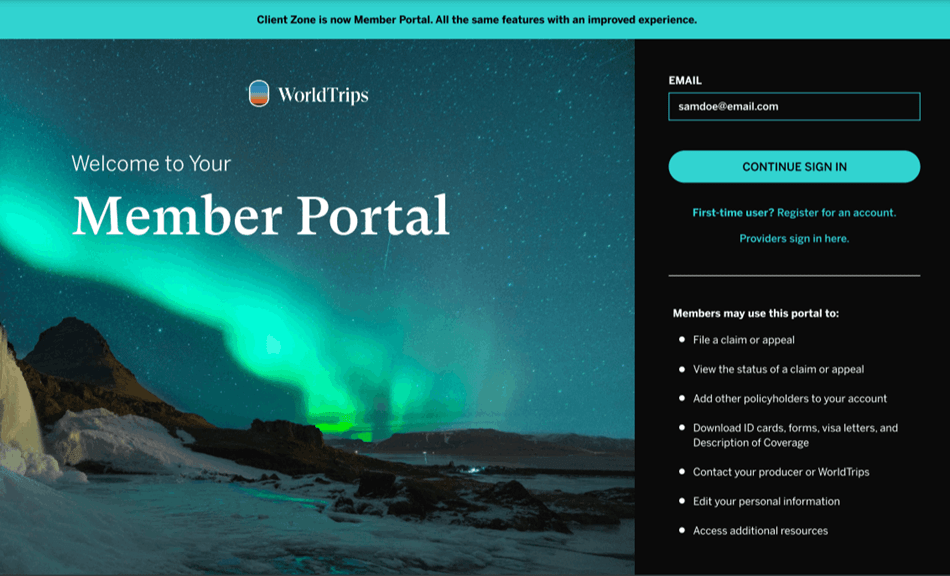
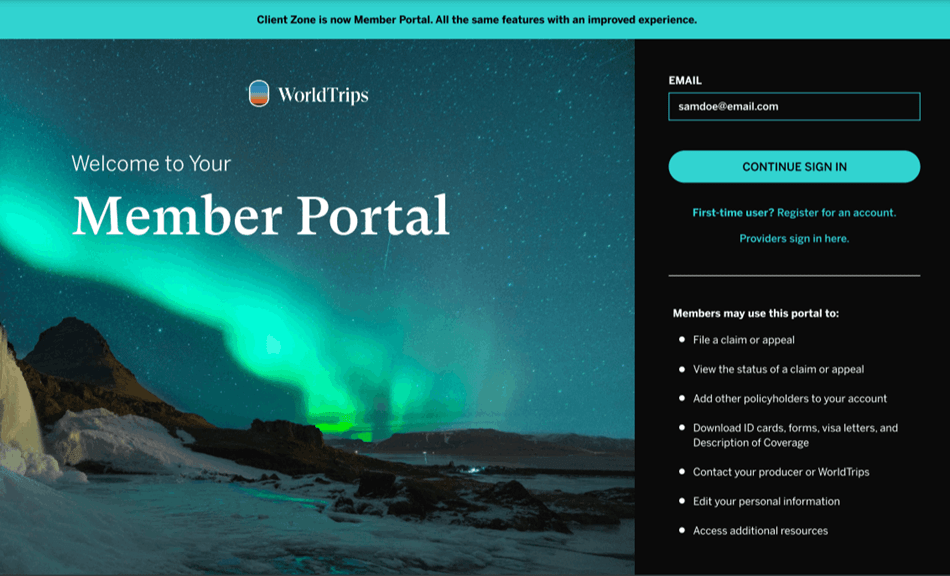
1. Visit Member Portal at https://worldtrips.my.site.com/MemberPortal. Enter the email address associated with your account and then click the “Continue Sign In” button.
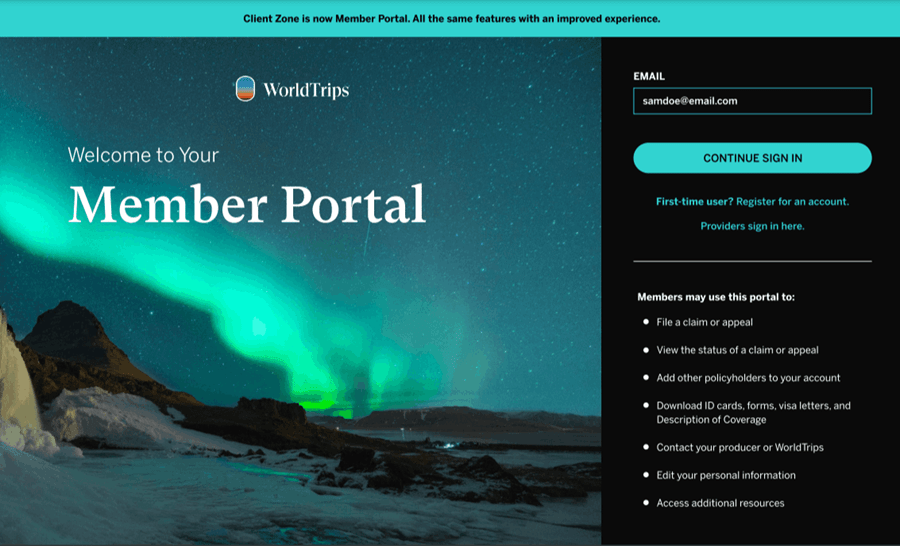
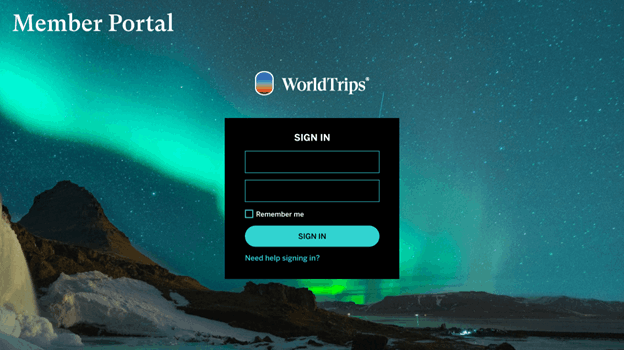
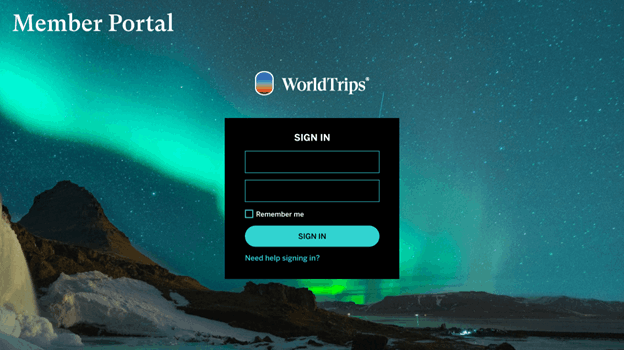
2. On the resulting Sign In page, enter your password below your email address. Then click the “Sign In” button.
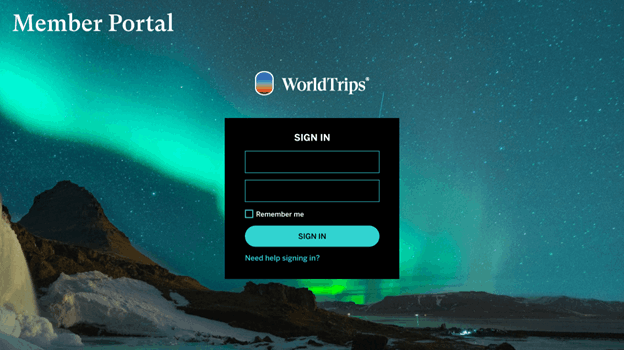
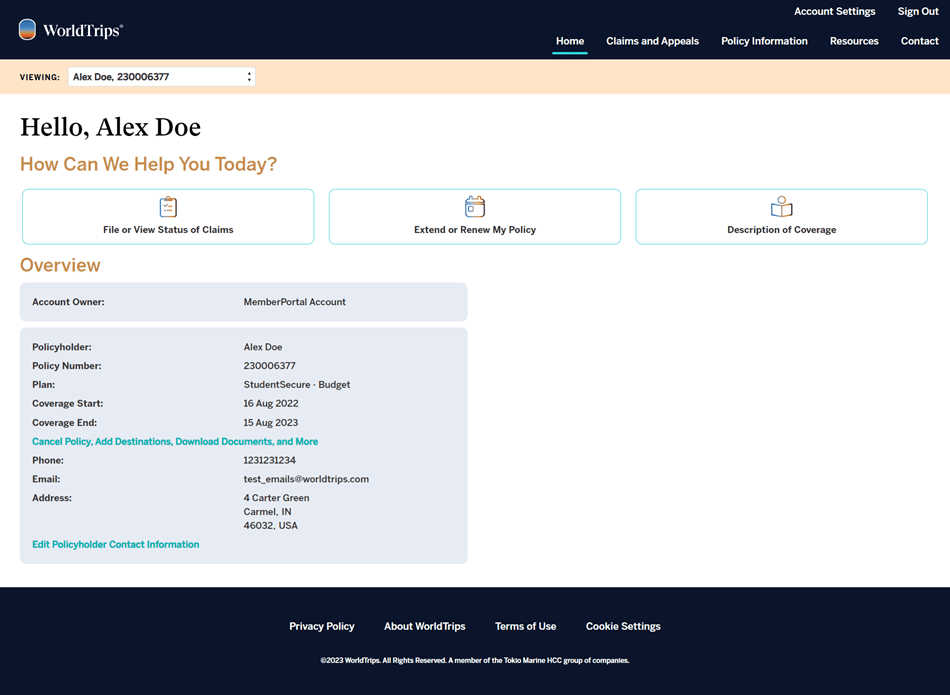
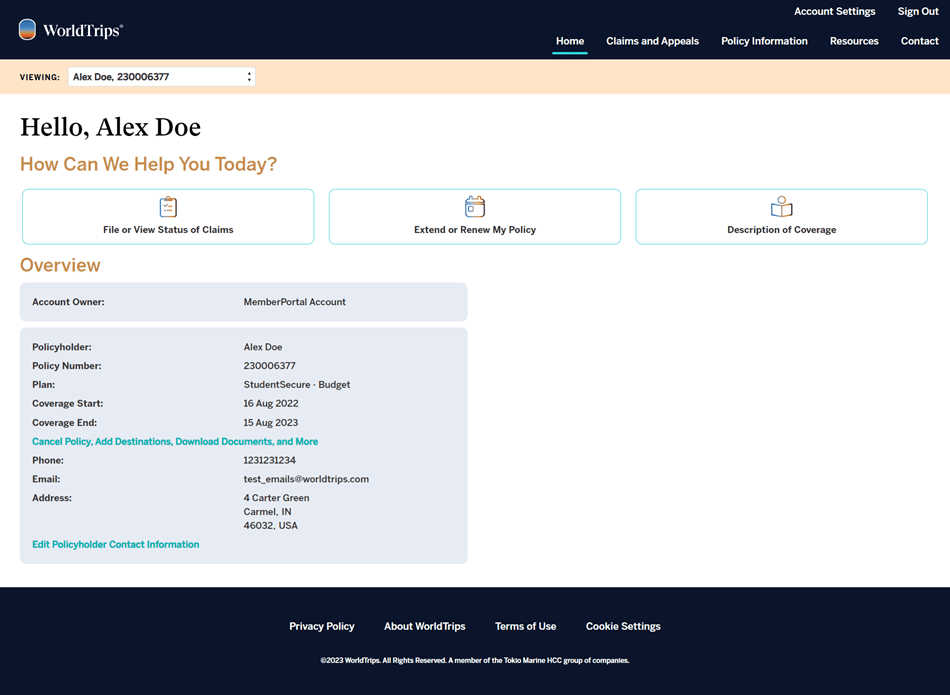
3. You will be presented with your Member Portal home page. Click “Claims and Appeals” in the main navigation menu at the top of the page.
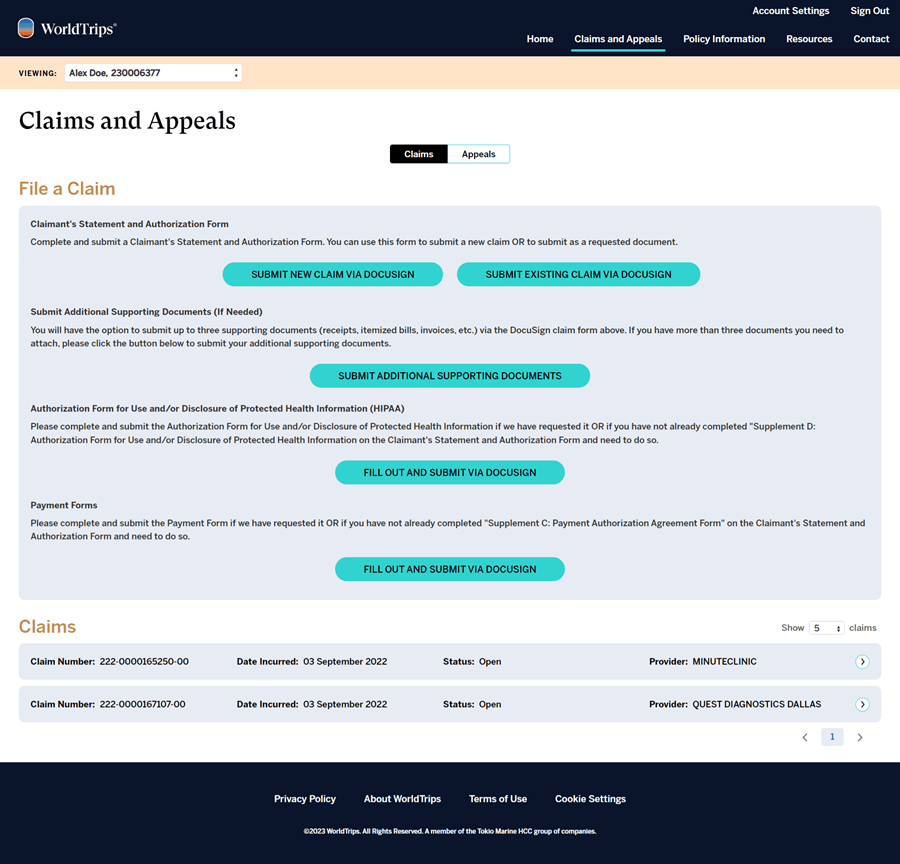
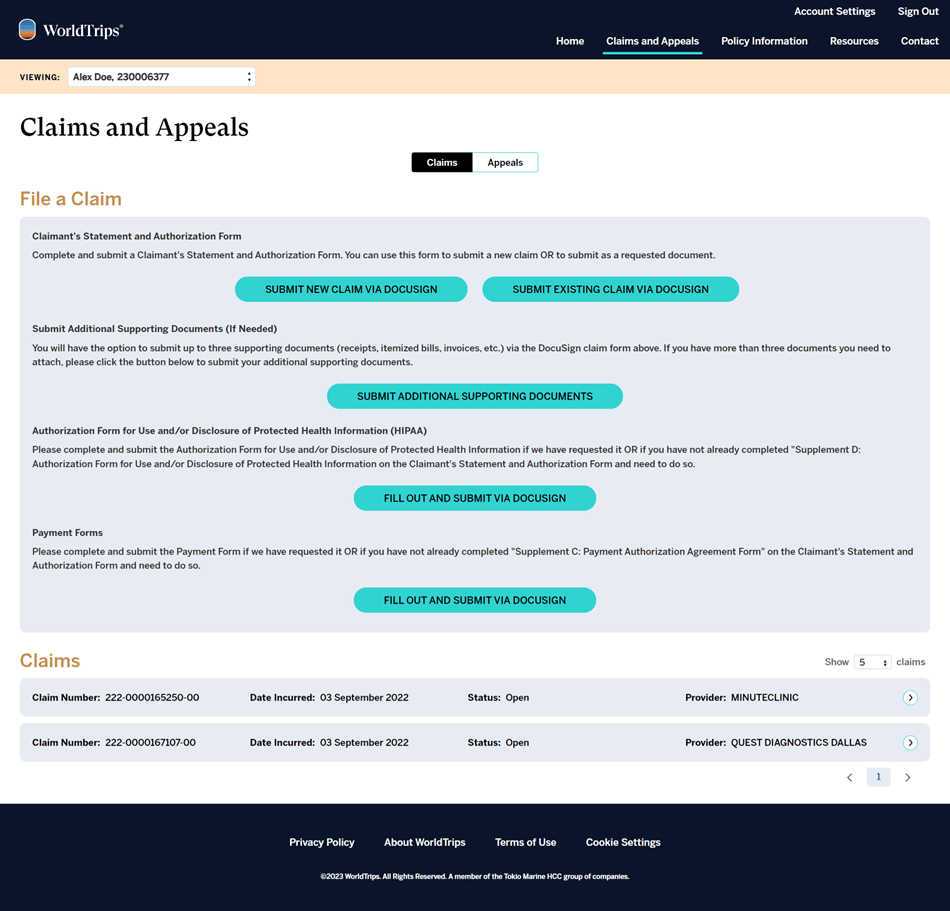
4. You will be presented with the Claims and Appeals page.
Don’t Have Access to the Claims and Appeals Page?
If you selected that you are not the insured or the insured’s legal guardian upon registration, you will not have immediate access to the Claims and Appeals page. Instead, you will see the Protected Health Information Authorization page. To gain access to this section of Member Portal, enter the insured’s email address and click the “Send Request” button.
The insured will receive an email with a link to complete, sign, and submit the HIPAA form via DocuSign. You will gain access to the Claims and Appeals section and will be able to submit a claim for the policyholder within 3-5 days of the date the policyholder completed and submitted the form.
To file a new claim via DocuSign, click the "Submit New Claim Via DocuSign" button under the "Claimant's Statement and Authorization Form" subheader in the "File a Claim" section.
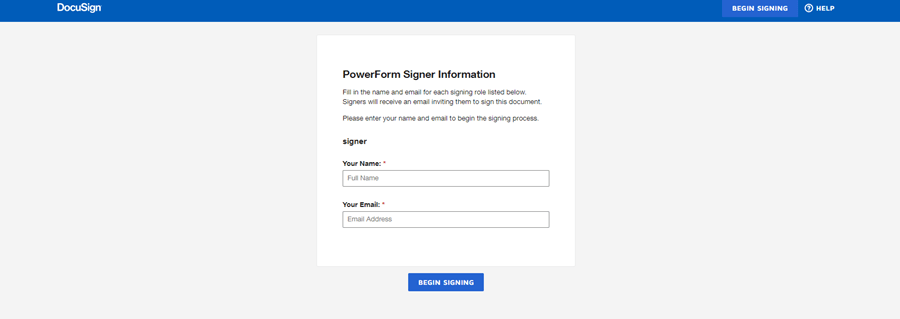
5. Enter your name and email address and click the “Begin Signing” button.
6. Click the white box next to “I agree to use electronic records and signatures.” Then click the yellow “Continue” button to the right.
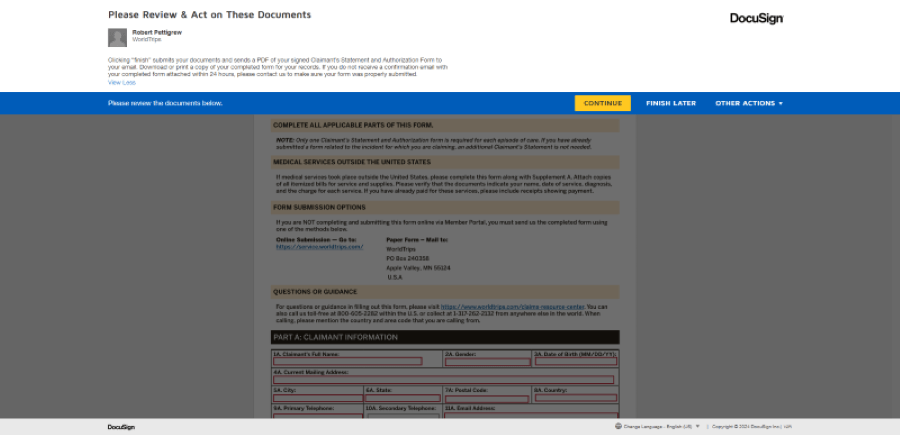
7. Fill in all the required information (as indicated by the red text boxes) and sign everywhere a signature is required (as indicated by the yellow “Sign” boxes).
Attach your supporting documents (medical records, receipts, itemized bills, etc.), if necessary, in the appropriate section via the yellow attachment boxes. If you have more than 3 attachments or exceed the 5MB attachment limit, see instructions for submitting additional documents below.
8. When you are done, click the yellow “Finish” button in the top righthand corner. Clicking “Finish” submits your documents and sends a PDF of your signed Claimant’s Statement and Authorization form to your email.
Download or print a copy of your completed form for your records. If you do not receive a confirmation email with your completed form attached within 24 hours, please contact WorldTrips to make sure your form was properly submitted.Need to Attach More Than 3 Supporting Documents OR Submit Additional Supporting Documents After You Have Already Submitted Your Claim Via DocuSign?
Return to the Claims and Appeals page of the Member Portal and click the “Submit Additional Supporting Documents” button under the “Submit Additional Supporting Documents (If Needed)” subheader in the “File a Claim” section.
You will land on the Submit Additional Supporting Documents page. Use the dropdown to choose your claim number. (If you have just submitted your Claimant’s Statement and Authorization form and do not yet have a claim number to select, you can still submit your documents without selecting a claim number.) Then upload your files and click the “Submit” button.
Once your documents have been successfully submitted, you will receive a confirmation email with your policy number, confirmation of the types of documents submitted (for a claim or appeal), your claim number (if selected), and the number of documents you submitted.
-
Click to view instructions
- Download the Claimant’s Statement and Authorization form here.
- Complete and sign the form.
- Visit worldtrips.com/customer-service and select “Submit a claim or appeal for your Atlas Travel, Atlas Premium, Atlas Group, Atlas MultiTrip, Atlas Nomads, or StudentSecure plan” under the “Actions” header.
- Click the “Submit Claim” button.
- Fill in the requested information on the Submit Claim Request form and upload the completed Claimant’s Statement and Authorization form, along with additional supporting documentation (medical records, receipts, itemized bills, etc.).
- Click "Submit."
- Download the Claimant’s Statement and Authorization form here.
-
Click to view instructions
- Download the Claimant’s Statement and Authorization form here.
- Print, complete, and sign the Claimant’s Statement and Authorization form. Mail the completed form, along with additional supporting documentation (medical records, receipts, itemized bills, etc.), to:
WorldTrips
Claims Department
PO Box 240358
Apple Valley, MN 55124
U.S.A.
WorldTrips is also happy to fax, e-mail, or mail the form to you upon request.
- Download the Claimant’s Statement and Authorization form here.
How the Direct Billing and Claims Reimbursement Process Works
We encourage providers to bill us directly, rather than requiring immediate payment from you. While we are always willing to pay providers directly for eligible claims, we cannot guarantee that the provider will accept your proof of insurance at the time of service.
If Providers Are Willing to Bill Us Directly:
-
Click to view instructions
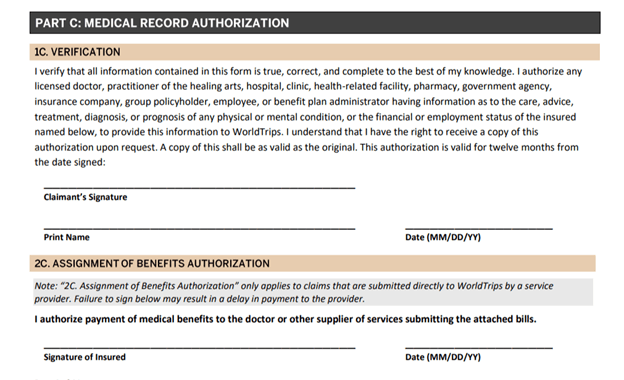
You must authorize the payment of medical benefits to the provider by signing and dating the section of the Claimant's Statement and Authorization form labeled "2C. Assignment of Benefits Authorization." You will find section "2C" under "Part C: Medical Record Authorization."
Providers must mail itemized bills, including diagnosis, to:WorldTrips
Claims Department
PO Box 240358
Apple Valley, MN 55124
U.S.A.
-
Click to view instructions
You must pay for medical treatment at the time of service and file a claim for reimbursement.
To file a claim, you must submit a completed Claimant’s Statement and Authorization form as well as all supporting documentation (original itemized bills, paid receipts, medical records, etc.) to WorldTrips.
You can complete and submit the Claimant’s Statement and Authorization form and supporting documentation in one of three ways:
- Via DocuSign in Member Portal (this is the most efficient method)
- Via the Customer Service page
- Via mail to:
WorldTrips
Claims Department
PO Box 240358
Apple Valley, MN 55124
U.S.A.
We encourage you to make copies of all documentation (Claimant’s Statement and Authorization form, medical records, bills, receipts, etc.) you send to us for your own records.
Need More Detailed Submission Instructions? Jump to the “How to File a Claim” section for additional instructions.
IMPORTANT NOTE
It is common for the claims department to request copies of medical records related to a claim or to your medical history. If you sought treatment outside the U.S., our claims department may require you to obtain the medical records related to your claim and submit them to us.
If we request additional information, further processing time may be necessary, depending on the response time of the parties from whom we requested the information.
We are not not able to pay a provider in advance of services rendered. While you may contact us at any given time to verify your benefits, this is not a guarantee that the charge is covered. We must have the ability to investigate a claim before determining whether it is eligible for payment.
How the Claims Review Process Works
A WorldTrips claims examiner will review the claim to determine if it can be processed or if more information is needed.
If more information is needed, the examiner will send a "Request for More Information" letter by mail to you and/or your medical provider.
You may respond to the "Request(s) for More Information" by taking one of the following actions:
- Upload the requested document(s) via Member Portal
- Upload the requested document(s) to an existing claim via the Submit Claim Request Form. You can access the form by visiting the Customer Service page and selecting “Submit a claim or appeal for your Atlas Travel, Atlas Premium, Atlas Group, Atlas MultiTrip, Atlas Nomads, or StudentSecure plan” under the “Actions” header. Then click “Submit Claim,” fill in the requested information, upload the requested documents, and click “Submit.”
- Mail the requested document(s) to:
WorldTrips
Claims Department
PO Box 240358
Apple Valley, MN 55124
U.S.A.
NOTE: If you or the medical provider do not respond within 45 days of the initial request for more information, the claim may be closed.
Wondering What Requests for More Information Have Been Sent?
You can see any requests for more information that WorldTrips has sent to you or a medical provider in the “Claims and Appeals” section of Member Portal. Sign into your account and click “Claims and Appeals” in the main navigation. Then scroll down under the “Claims” header to view your claims.
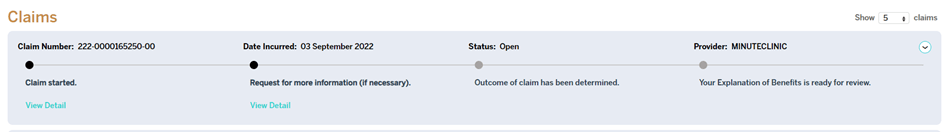
Click the arrow to the right of the claim that you would like to view. Click “View Detail” under each step to see additional details about where your claim is in the review process. If WorldTrips has sent a letter to you or a medical provider, you will be able to click to download the letter here.
If WorldTrips has requested additional information from you, clicking the link in the timeline will take you to a page where you can download the letter we sent and submit the requested information. You will receive a confirmation email upon the submission of any requested documents and see a confirmation message in the claim timeline under the initial letter request.
IMPORTANT! Remember that you must add your policy to Member Portal to see claims associated with the policy. Click here to jump to the “How to Add a Policy to Member Portal” section of this guide for detailed instructions.
-
Click to view instructions
To view your claim status via Member Portal, you will first need to register for a Member Portal account. Here’s how:
1. Visit Member Portal at https://worldtrips.my.site.com/MemberPortal.
2. Under “Continue Sign In” click “First-time user? Register for an account.”
3. On the Register page, enter the email address you wish to use to sign into your account. This email does not need to match the email address associated with your policy.
Enter your policy number and select whether or not you are the insured or the insured’s legal guardian. Enter the insured’s first and last name as entered on the policy. (You can see how the insured’s name was entered on your ID card and fulfillment documents that were sent to you upon purchase.)
Enter the insured’s date of birth. Then choose a password. Follow the password instructions noted on the page.
Read and agree to the terms and conditions by checking the box. Then click the “Continue” button.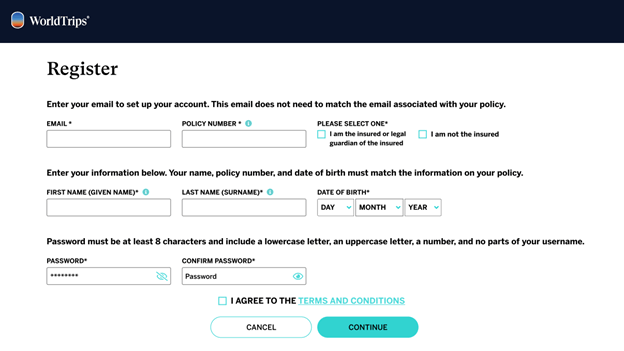
4. You will be taken to the Sign In page. Enter the email address and password you used to register your account and click “Sign In.”
5. To add an additional layer of security when signing into your account, you will be prompted to choose your preferred multifactor authentication method.
Options Include:
a. Okta Verify - Click "Setup" if you wish to use a push notification sent to the mobile app
b. SMS Authentication* - Click "Setup" if you wish to enter a single-use code that is sent to your mobile phone
c. Voice Call Authentication* - Click "Setup" if you wish to follow voice instructions via phone
d. Security Question - Click "Setup" if you wish to answer a security question
*Please be sure to use a method which you will have continual access to on your travels. Do not use phone numbers that will not work outside of your current service area.
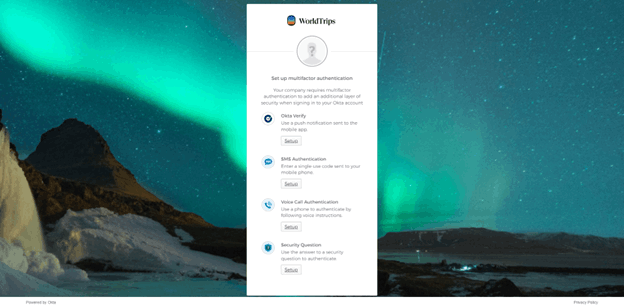
6. Follow the setup instructions of your chosen multifactor authentication method. Then click “Finish.”
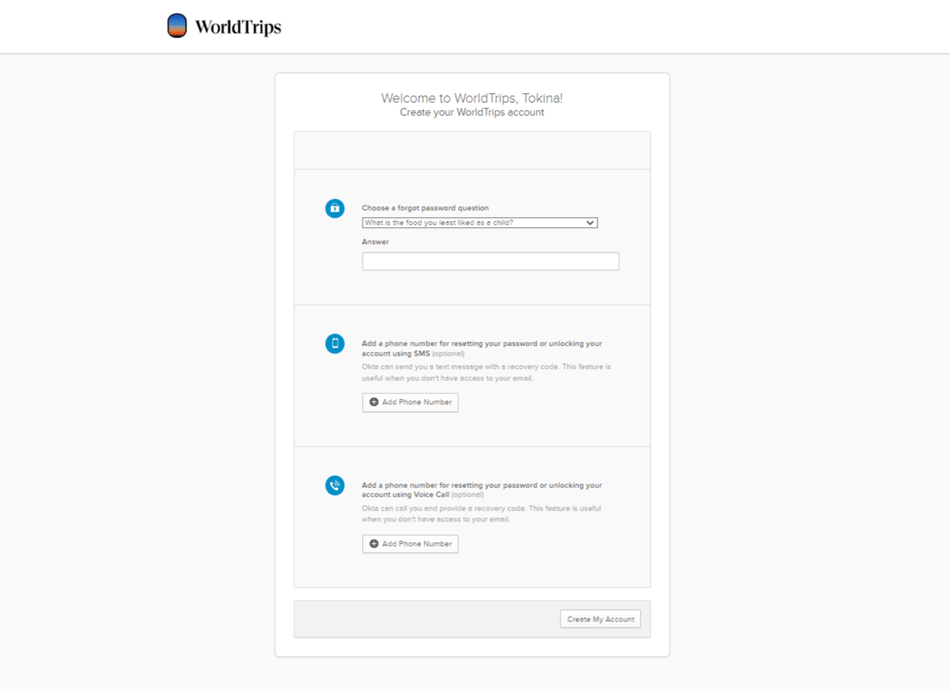
7. On the resulting page, choose a "Forgot Password" question. Make sure you select a question with only one correct answer that is easy to remember.
Type the answer into the blank box below "Answer." You will need this answer to access your account if you ever forget your Member Portal password and need to reset it.
You may also choose to add a phone number for resetting your password or unlocking your account using SMS text message or a voice call if you don’t have access to your email.
Click "Create My Account."
-
Click to view instructions
You will need to add each policy you wish to view in Member Portal. Adding a policy will allow you to view and edit your policy details, extend or renew your policy (if eligible), view the status of your claim, and more.
1. To add a policy, sign into your Member Portal account.
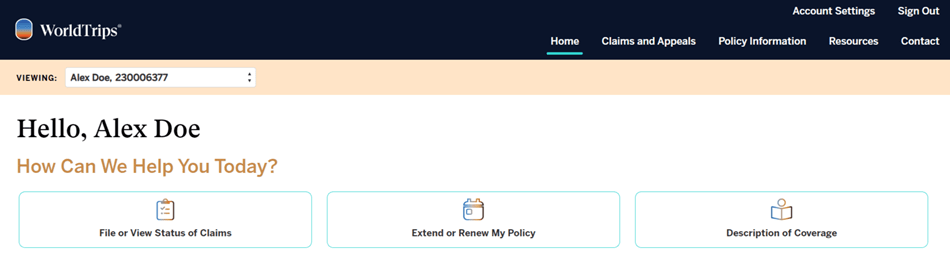
2. From your home page, click into the white box in the top lefthand corner of the page next to “Viewing” (below the WorldTrips logo). Click “+ Add Policy.”
3. Fill in the policy number for the plan you wish to add to your account. Select whether or not you are the insured or legal guardian of the insured. Add the first name, last name, and date of birth for the insured member on the policy. This must match the information on the policy. Then click the “Add Policy” button.
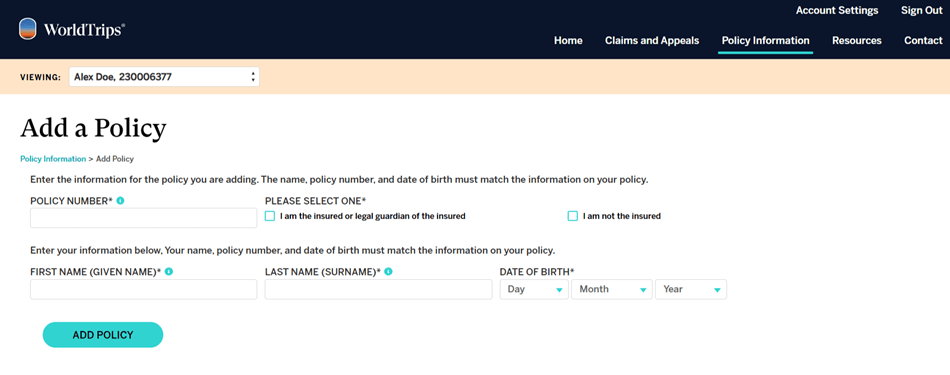
Once you have successfully added your policy, you should be able to see it in your Member Portal account.
-
Click to view instructions
But First, Did You Register for a Member Portal Account?
Visit the Member Portal welcome page at https://worldtrips.my.site.com/MemberPortal and click “First-time user? Register for an account” below the “Continue Sign In” button. Follow the instructions to create your Member Portal account. If you need additional help, click here to view registration instructions.
Haven’t Yet Added Your Policy to Your Member Portal Account?
You will need to add your policy to your Member Portal account before you will be able to see your claim status in Member Portal. Click here to jump to the “How to Add a Policy to Member Portal” section of this guide.
1. On the Member Portal welcome page, enter the email address you used to register your account and click the “Continue Sign In” button.
2. On the resulting Sign In page, enter the password you entered when you created your account below your email address. Click "Sign In."
3. From your Member Portal home page, click “File or View Status of Claims” under the “How Can We Help You Today?” header.
4. This will take you to the Claims and Appeals page. (You can also get here by clicking “Claims and Appeals” in the main navigation.) Scroll down and find your claim(s) under the “Claims” header.
Don’t See Your Claim?
You will need to add your policy to your Member Portal account before you will be able to see your claim status on the Claims and Appeals page. Click here to jump to the “How to Add a Policy to Member Portal” section of this guide.
Don’t Have Access to the Claims and Appeals Page?
If you selected that you are not the insured or the insured’s legal guardian upon registration, you will not have immediate access to the Claims and Appeals page. Instead, you will see the Protected Health Information Authorization page. To gain access to this section of Member Portal, enter the insured’s email address and click the “Send Request” button.
The insured will receive an email with a link to complete, sign, and submit the HIPAA form via DocuSign. You will gain access to the Claims and Appeals section and will be able to submit a claim for the policyholder within 3-5 days of the date the policyholder completed and submitted the form.
5. You will be able to see your claim number, the date the claim was incurred, the claim status, and the relevant provider.
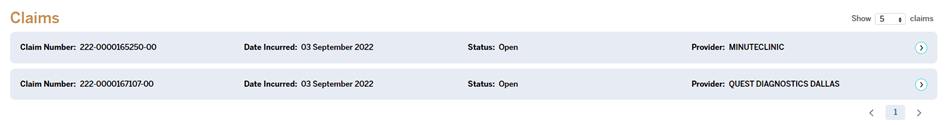
6. Click the arrow to the right of the claim you wish to view to see more information for the claim, including where your claim is in the claim process (whether it has been started, whether there has been a request for more information, whether the outcome of the claim has been determined, and whether your Explanation of Benefits is ready for review).
You can click “View Detail” under each completed step to see more information.
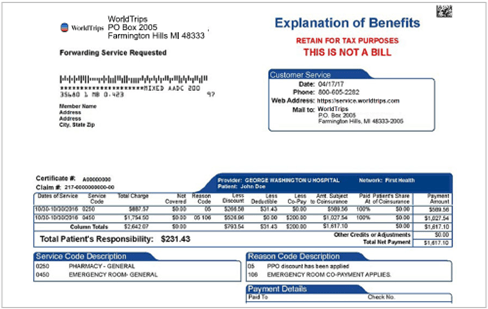
7. When finalized, each claim will have an Explanation of Benefits (EOB) associated with it. To view the EOB for the claim, click “Download your Explanation of Benefits.” Then open the downloaded PDF to view your EOB.
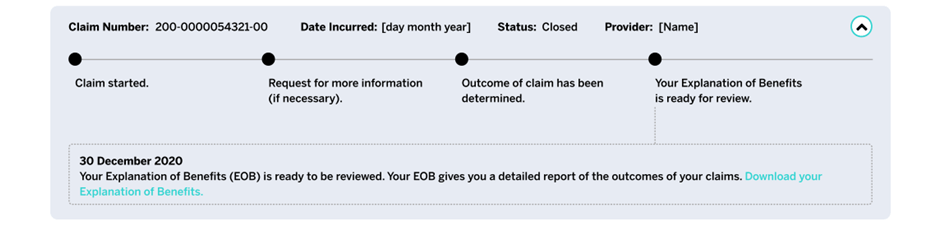
An example EOB is shown below. It displays the various data elements contained within a standard EOB from WorldTrips.
-
Click to view instructions
You can complete, sign, and submit the Claimant Appeal Request form online via Member Portal, our self-service portal for policyholders.
Have You Registered for a Member Portal Account?
To access Member Portal, you will first need to register an account. Please refer to the "How to Register for a Member Portal Account" section of this document for registration instructions.
If you have already registered your account, follow the instructions below.
Haven’t Yet Added Your Policy to Your Member Portal Account?
You will need to add your policy to your Member Portal account before you will be able to appeal your claim in Member Portal. Click here to jump to the “How to Add a Policy to Member Portal” section of this guide.
1. Visit Member Portal at https://worldtrips.my.site.com/MemberPortal. Enter the email address associated with your account and then click the “Continue Sign In” button.
2. On the resulting Sign In page, enter your password below your email address. Then click the “Sign In” button.
3. You will be presented with your Member Portal home page. Click “Claims and Appeals” in the main navigation menu at the top of the page.
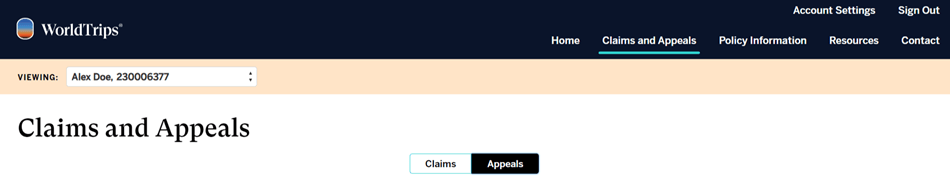
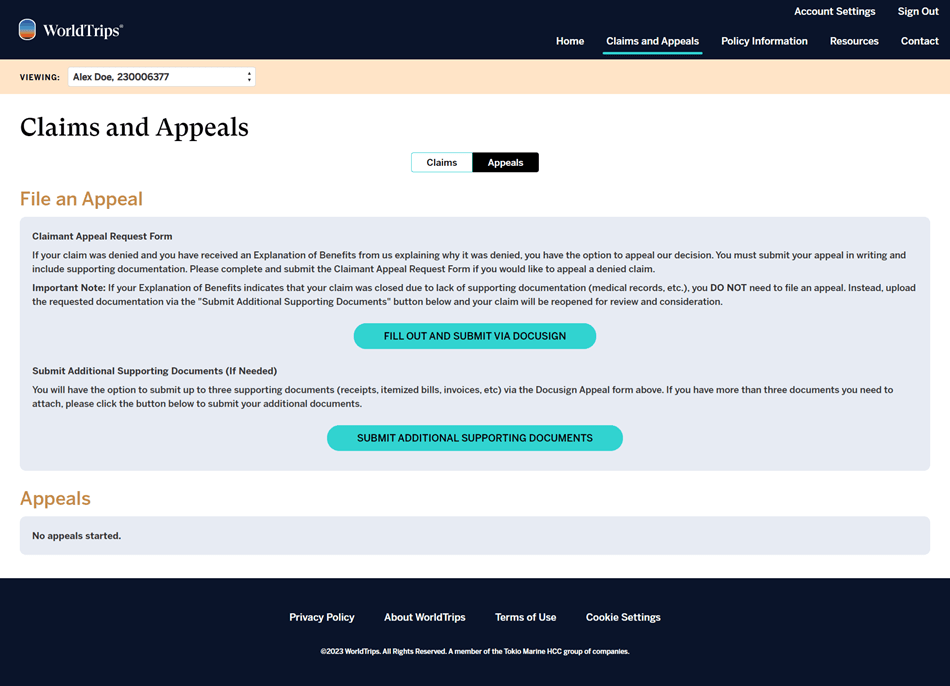
4. You will be presented with the Claims and Appeals page. Switch the toggle at the top of the page under the “Claims and Appeals” header from “Claims” to “Appeals.”
Don’t Have Access to the Claims and Appeals Page?
If you selected that you are not the insured or the insured’s legal guardian upon registration, you will not have immediate access to the Claims and Appeals page. Instead, you will see the Protected Health Information Authorization page. To gain access to this section of Member Portal, enter the insured’s email address and click the “Send Request” button.
The insured will receive an email with a link to complete, sign, and submit the HIPAA form via DocuSign. You will gain access to the Claims and Appeals section and will be able to submit a claim for the policyholder within 3-5 days of the date the policyholder completed and submitted the form.
5. To file an appeal via DocuSign, click the “Fill Out and Submit Via DocuSign” button under the “Claimant Appeal Request Form” subheader in the “File an Appeal” section.
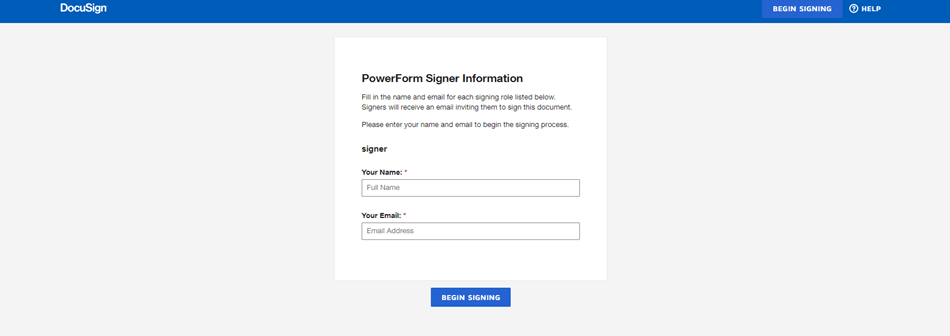
6. Enter your name and email address and click the “Begin Signing” button.
7. Click the yellow “Continue” button to the right.
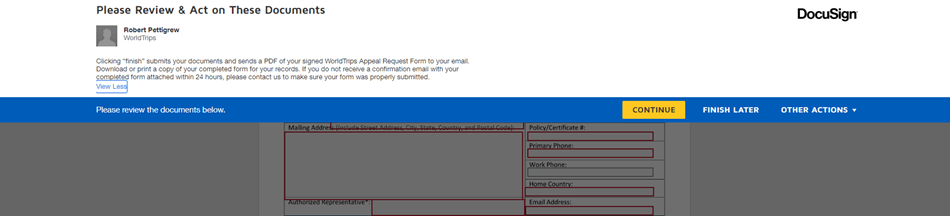
8. Fill in all the required information (as indicated by the red text boxes) and sign everywhere a signature is required (as indicated by the yellow “Sign” boxes).
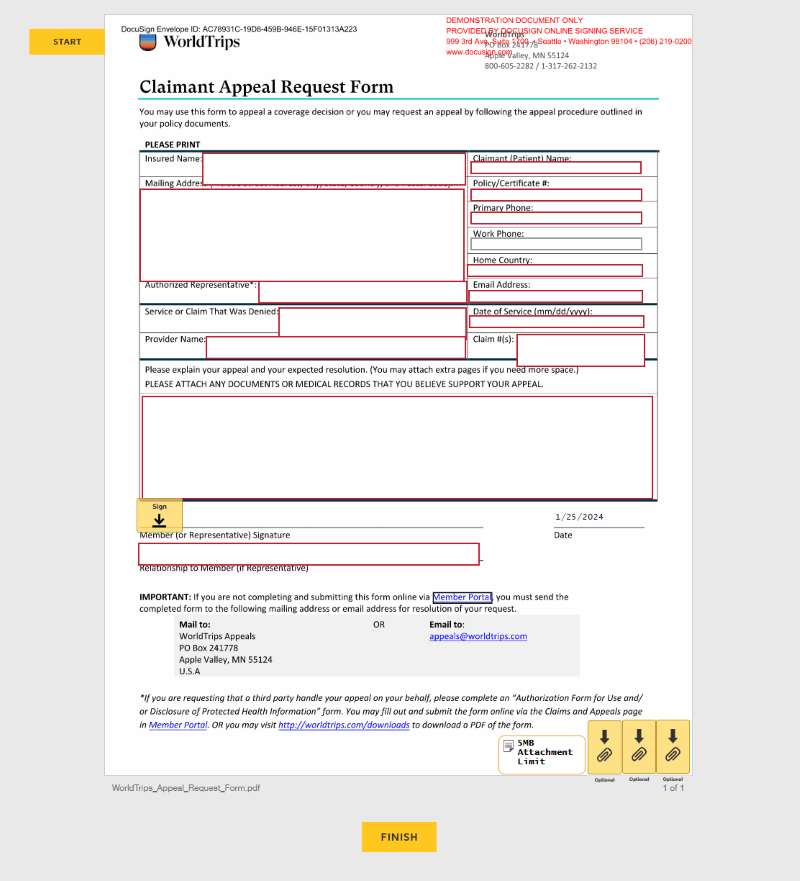
Attach your supporting documents (medical records, receipts, itemized bills, etc.), if necessary, at the bottom righthand corner of the page via the yellow attachment boxes. If you have more than 3 attachments or exceed the 5MB attachment limit, see instructions for submitting additional documents below.
9. When you are done, click the yellow “Finish” button at the bottom of the page. Clicking “Finish” submits your documents and sends a PDF of your signed Claimant Appeal Request Form to your email.
Download or print a copy of your completed form for your records. If you do not receive a confirmation email with your completed form attached within 24 hours, please contact WorldTrips to make sure your form was properly submitted.Need to Attach More Than 3 Supporting Documents OR Submit Additional Supporting Documents After You Have Already Submitted Your Appeal Via DocuSign?
Return to the Claims and Appeals page of the Member Portal and switch the toggle below the “Claims and Appeals” header from “Claims” to “Appeals.” Click the “Submit Additional Supporting Documents” button under the “Submit Additional Supporting Documents (If Needed)” subheader in the “File an Appeal” section.
You will land on the Submit Additional Supporting Documents page. Use the dropdown to choose your claim number. Then upload your files and click the “Submit” button.
-
Click to view instructions
- Visit worldtrips.com/customer-service.
- Select “Submit a claim or appeal for your Atlas Travel, Atlas Premium, Atlas Group, Atlas MultiTrip, Atlas Nomads, or StudentSecure plan” under the “Actions” header.
- Click “Submit Appeal.”
- Fill in the requested information on the Claimant Appeal Request Form and upload additional documentation that supports your reasoning and position (medical records, receipts, itemized bills, etc.).
- Click "Submit."
- Visit worldtrips.com/customer-service.
-
Click to view instructions
- Download the Claimant Appeal Request Form here.
- Fill out the form and email it, along with additional documentation that supports your reasoning and position (medical records, receipts, itemized bills, etc.), to [email protected].
OR
Mail the form and supporting documents to:
WorldTrips Appeals
PO Box 241778
Apple Valley, MN 55124
U.S.A - Download the Claimant Appeal Request Form here.
-
Click to view instructions
- Write a letter of appeal following the appeal procedure instructions outlined in your policy documents/certificate of coverage.
- Email this written letter of appeal, along with additional documentation that supports your reasoning and position (medical records, receipts, etc.), to [email protected].
OR
Mail the form and supporting documents to:
WorldTrips Appeals
PO Box 241778
Apple Valley, MN 55124
U.S.A
Please note that submission of the appeal will lead to re-evaluation of your claim but does not guarantee that the initial benefit determination will be altered. - Write a letter of appeal following the appeal procedure instructions outlined in your policy documents/certificate of coverage.
KHE2FFFYH6SP-971744701-998
WorldTrips is a service company and a member of the Tokio Marine HCC group of companies.
WorldTrips’ Atlas Journey, Atlas Cruiser, and Atlas On-The-Go trip protection insurance products are underwritten by Tokio Marine HCC’s U.S. Specialty Insurance Company (USSIC). USSIC is a Texas-domiciled insurance company operating on an admitted basis throughout the United States.
In the State of California, operating as WorldTrips Insurance Services. California Non-Resident Producer License Number: 0G39705
WorldTrips’ Atlas Travel Series, Atlas Nomads, and StudentSecure international travel medical insurance products are underwritten by Lloyd's. WorldTrips has authority to enter into contracts of insurance on behalf of the Lloyd's underwriting members of Lloyd's Syndicate 4141, which is managed by HCC Underwriting Agency, Ltd.